
The information and resources in this article are not a substitute for professional advice. If you have concerns about your child, seek help and support from an appropriately qualified practitioner.
What is a tongue-tie?
Most simply put, tongue-tie or Ankyloglossia, is a common condition present at birth that restricts the tongue’s ability to move as needed. Studies suggest 1 in 10 babies may be born with a restrictive membrane under their tongue.
It’s important to note, everyone is born with a piece of tissue (lingual frenulum) under their tongue that tethers the tongue to the bottom of the mouth. Same with the upper lip. However, a tongue-tie is an unusually short, thick, or tight band of tissue restricting the tongue from a typical range of motion required for feeding, swallowing, speech, or typical development. To have a tongue-tie or lip-tie release, there must be a physical abnormality AND functional concern.
A tongue-tie is only one type of Tethered Oral Tissue (TOT). There are actually 7 places tissue can be restricted in the mouth:
- Under the tongue
- Top lip
- Bottom lip
- Top left cheek
- Top right cheek
- Bottom left cheek
- Bottom right cheek




Why are tongue-ties a little complicated and misunderstood?
-
Tongue-ties are only treated when there is a functional need, and functional needs vary person to person.
Some children may have restricted frenulum tissue, but do not have functional issues and therefore no treatment is needed. For others, the impact can be substantial. Treatment is recommended only in individuals with symptoms. Tongue-tie can be treated at all ages, one day after birth or into adulthood, if and when symptoms appear.
-
Tongue-ties are not always obvious.
There’s different types of tongue-ties. Some tongue-ties are more easily seen at the front of the tongue blade (anterior restriction), but other times the tongue will be tethered father back and not as easily observed (posterior restriction).
-
Parents may not know to seek a specialized preferred provider with experience and expertise in tongue-ties.
Often a parent with concerns starts by asking a generalized physician or other healthcare provider who does not have sufficient knowledge to properly diagnose or treat a tongue-tie. Preferred providers for tongue-tie include the following who have specifically gained specialized training and education beyond their general practice: pediatric dentists, ENTs, international board certified lactation consultants (IBCLC), speech-language pathologists (SLP), and oromyofacial therapists.
-
We’re still learning how important the tongue is in the body.
Tongue-tie is not a new trend; there are referenced made in medical texts dating back to the 17th century. However, because there is not a conceptual framework for consistent diagnosis and treatment across medical fields, the research is difficult to apply across the board. Recommendations can vary, which can be confusing for caregivers. Also, tongue-tie is not just related to breastfeeding, but can actually impact the whole body function.
What causes tongue-tie?
The exact cause of tongue-tie is unknown. Studies indicate it is hereditary, so it is common in families and is more common in boys.
How do I know if there is a tongue-tie?
Most often, tongue-ties are discovered when breastfeeding or an infant has trouble feeding. However, there are other signs and symptoms of tongue-tie as well. Not all signs or symptoms must be present to be diagnosed; most common are listed below:
For breastfeeding mothers:
- Misshapen nipples during/after feeding (ridged, blanched, “lipstick-shaped”)
- Sore, blistered, cracked, bleeding, bruised nipples
- Painful breastfeeding not solved by positioning strategies
- Mastitis or blocked milk ducts
- Low milk supply
- Over supply of milk
- Exhaustion from frequent/constant feeding
- Distress from breastfeeding relationship
- Weaning from breastfeeding
For infants:
- Restricted tongue movement
- Tongue may appear heart-shaped or forked, especially when crying
- Tongue may appear to have a bowl-shape or dimple in the middle, especially when crying
- May or may not be able to stick tongue past the lips
- May or may not observe tongue cupped to form a bowl shape when crying
- Difficulty breastfeeding
- Inability to open mouth wide when latching to the breast resulting in biting/grinding movements on the nipple
- Clicking noises when feeding
- Milk spilling from mouth during feeds
- Coughing on milk flow
- Difficulty staying latched
- Falling asleep at the breast
- Frequent or very long feeds
- Lip blisters
- Colicky, Irritable during or after feeding (inefficient feeding)
- Excessive early weight loss, poor weight gain (inefficient feeding)
- Reflux (vomiting after feeds due to swallowing air during feeds as result of poor latch)
- Inability to take a pacifier
For older children and adults:
- Restricted tongue movement
- Tongue may appear heart-shaped or forked, especially when lifting the tongue up
- May or may not be able to stick tongue past the lips
- May or may not observe tongue cupped to form a bowl-shape or dimple when lifting the tongue up
- Feeding difficulties
- Picky eating
- Reflux (vomiting after feeds)
- Difficulty eating certain textures or choking on liquids
- Difficulty bottle or cup feeding
- Difficulty spoon feeding
- Difficulty chewing and swallowing
- Messy eating, requires many liquid washes, drooling
- Speech difficulties (unable to lift tongue to top of mouth to produce certain sounds)
- Dental issues (unable to use tongue to clean teeth)
- Cavities
- Gum disease
- Crowded teeth
- Chronic bad breath
- Chronic dry lips
- Atypical facial development
- Narrow and high oral palate
- Narrow or misaligned jaw
- Small sinus cavities
- Sleep apnea/sleep disturbance, snoring
- Neck, back, and/or facial pain
- Headaches and/or migraines
- Clicking, teeth grinding/clinching, and/or pain in jaw (TMJ)
- Sinus problems
- Mouth breathing
- Improper lingual rest (tongue pushing against teeth or laying in bottom of mouth)
- Poor posture (head forward, shoulders tense)
- Extended thumb sucking
- Challenges with other activities like licking an ice cream cone, kissing, playing instruments, etc.
Why should I consider a tongue-tie release or treatment for TOTs?
If you have concerns with feeding, speaking, breathing, or sleeping, an assessment for tongue-tie is recommended. Many people do not realize, in individuals with functional deficits, the restricted tongue can be associated with a variety of disorders and issues later in life. Feeding difficulties in infancy and childhood are related with many other medical disorders that can impact development.
Untreated tongue-tie can result in sleep disorders, dental and oral hygiene issues, facial development abnormalities, picky eating, speech disorders, TMJ/tension in neck and face, headaches or migraines, sinus problems, and reflux later in lifeM





Click a question below to learn more about tongue-ties.
Tongue-tie should be diagnosed based on physical abnormality AND functional need. Looking at a picture of a tongue does not offer information about how successful the child is in feeding or speaking. Some practitioners use location of restriction to determine severity or class of tie, but ultimately it should always be based on the primary concerns and functional ability.
Although newborns are screened for a variety of abnormalities during the routine birth assessment, this often does not include assessment for tongue-tie. Unfortunately, it is highly unlikely a generalized pediatrician or nurse will have specific training in tongue-tie assessment and therefore will miss the restriction or incorrectly diagnose. Although it is not typically routine for every birth, most hospitals can offer certified lactation consultants when requested.
Preferred providers for tongue-tie include the following who have specifically gained specialized training and education beyond their general practice: pediatric dentists, ENTs, international board-certified lactation consultants (IBCLC), speech-language pathologists (SLP), and oromyofacial therapists.
When a tongue-tie is suspected, a referral to a specialized preferred provider both skilled and knowledgeable in feeding and tongue-tie is essential. The assessment should include a thorough birth and breastfeeding/feeding history with present concerns highlighted (functional needs). The professional should also observe a feeding if at all possible and assess suck and tongue function. This typically involves putting a finger in the child’s mouth to evaluate how the infant uses their tongue to coordinate suck, swallow, and breathe patterns necessary for feeding. Additionally, the tongue is assessed for range of motion or how the tongue moves side to side and up and down.
Correct examination of infants requires the infant to be placed on the examiner’s lap with the infant’s head facing the same direction as the person evaluating and the infant’s feet in the caregiver’s lap. Assessment in a different position will likely lead to an incorrect or missed diagnosis.

A recommended treatment plan could involve the following steps:
- Assessment of feeding and functional concerns and treatment trial if necessary.
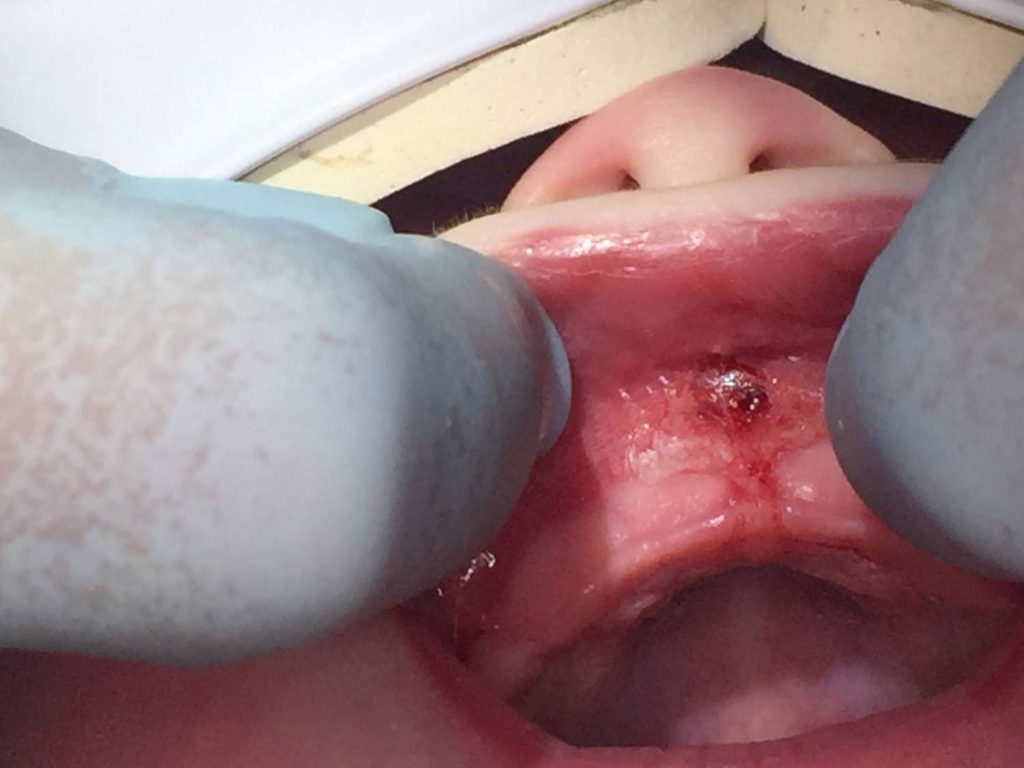
- Tongue-tie release by practitioner resulting in diamond-shaped cut
- Wound management by caregiver
- Feeding therapy (speech-language pathologist) or lactation support, if needed
- Other therapy as needed, such as Oral Myofunctional Therapy, physical therapy, occupational therapy, chiropractic, Cranial Sacral Therapy, Osteopathic Manipulative Therapy, or massage therapy.
Tongue-tie release, known as a frenotomy or frenectomy, is a small incision into the connective tissue to allow more movement of the tongue, lips, and/or cheeks. The practitioner may use sterile scissors or water laser to clip or release the restricted tissue to allow for more range of motion.
This procedure is typically done in an office setting with only local analgesia or nothing at all. There is very little risk and usually very effective in improving function with follow-up care and supportive therapy. Talk with your preferred provider to learn more about which method they use for release. Most preferred providers now use a laser frenectomy, as it is quick and effective, has a lower risk of infection, reduced post-surgical pain and swelling.
Uncommon risks of tongue-tie release procedure include:
- Recurrence – most common complication due to improper post-operative wound management (stretches/exercise) or inefficient release the first time
- Minor bleeding
- Infection
- Pain
- Damage to tongue and salivary ducts in the mouth
A tongue-tie release is the act of cutting the tissue as needed for functional movement.
Tongue-tie revision is when a secondary release is required due to reattachment or lack of complete release.
The mouth heals relatively quickly in comparison to other parts of the body. Also, open oral wounds contract towards the center as it is healing. However, in order for the tissue not to reattach, we need to slow the healing process and keep the wound open in order for the wound to heal from the inside first. Your preferred provider will provide specific instructions for exercises and care following the procedure. It may include stretching the area, massaging the wound, or moving the tongue. These stretches are typically recommended for 2-3 weeks following the procedure.
More information on what to expect with wound management.
Some people report they see immediate results after the tongue-tie release, but for others it may take up to 2-3 weeks to re-learn swallowing motor patterns. However, if wound management is not successful and tongue reattaches, results will naturally take longer.
Imagine, as a runner, you had to run every race with your shoes tied together. You could probably finish the race eventually, but it wouldn’t be very graceful. Then on day, you untie the knot and now are able to run without restriction, but you’ve never ran like this before. You need to re-learn how to run in this new way. It takes time and effort to re-learn, but eventually you are able to run gracefully and finish the race faster.
This is how it feels to have a tongue-tie release. The child likely has learned maladaptive compensatory strategies to overcome the restriction. After the tongue is released, the muscles do not have the patterns established for free movement and must learn new patterns for eating and speaking. Now that there is no abnormal tissue tethering the tongue, it may even rest in a new position in the mouth during breathing and sleeping.
Therapy can be extremely beneficial to helping establish these new patterns as well as assist in wound care immediately following the procedure to ensure reattachment does not happen.
This is why therapy is so important. The child has learned to compensate with a restricted tongue and now has full range of motion, but isn’t practiced in using it. It can take a few weeks for the child to learn how to use their tongue during feeding.
No, this is not true. Even in utero, a baby learns to swallow. After birth, we swallow between 500-700 times a day. If our tongue is restricted and unable to swallow correctly, we will learn to use compensatory strategies. The habit of incorrect swallowing pattern is reinforced and may contribute to atypical development and issues later in life.
No, weight gain is not the only sign of a successful feeding relationship. If you have concerns or see any of the red flags listed above, you should seek a tongue-tie assessment from a preferred provider.
International Association of Tongue-Tie Professionals (IATP) -FAQs and research
Dr. Lawrence Kotlow, DDS -research and articles
Dr. Bobby Ghaheri, MD -research and articles
Alabama Tongue-Tie Center -videos
Tongue-Tie Book – free download

I just found your website. I am a general dentist of 40+ years, have been treating TOTS since 1984.
Your site is excellent! Very informative. May I refer by patients to it?
Yes, of course. Thank you!
It helped when you wrote that tongue-tie is more common among boys. My friend wants to treat her child’s tongue tie. I think it’s best for her to look for a dental clinic that specializes in tongue releases.
Definitely tell her to have a doctor trained in it and not do it herself. Youe mouth is full of germs . All I have to do is suck my finger if I have pulled a hangnail off and it’s bleeding and it gets infected.
I never took into account the fact that untreated tongue tie issues can also affect the sleep, dental, oral, facial, speech, and other aspects of an individual. So it’s important that my sister immediately gets her daughter diagnosed to see if her daughter needs to undergo tongue-tie surgery. Because we all noticed that there is something different with how her daughter eats or makes sounds as a baby.
Your information is very helpful. It is very frustrating that for most families, the procedure and follow up is not covered by insurance.